Congenital Brown Syndrome (Superior Oblique Tendon Sheath Syndrome)
Brown syndrome is a problem with a tendon that attaches to the eyeball. The tendon is called the superior oblique muscle tendon. In Brown syndrome, this tendon can’t move freely. This limits the eye’s movement. Brown syndrome is a rare disorder. It is usually present at birth (congenital). In some cases, it’s acquired later in life.
Understanding eye movement
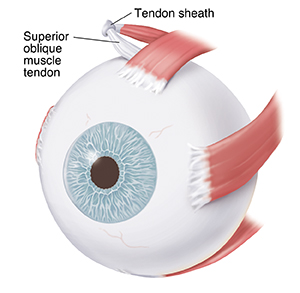
Eye movement is done with muscles and tendons attached to the eye. The superior oblique muscle tendon attaches to a small eye muscle. This muscle pulls the eye toward the middle, pulls the eye to look down, and rotates the eye. The superior oblique muscle tendon moves through a ring of tissue that surrounds it. The ring of tissue is called the tendon sheath.
What causes congenital Brown syndrome?
Congenital Brown syndrome is caused by problems with the superior oblique muscle tendon or its sheath. The muscle tendon or its sheath might be too short or thick. Experts don't know what causes Brown syndrome. It may be passed down from parent to child. Brown syndrome that's acquired is rare. But it can happen after surgery or trauma, or with an inflammatory disease. Your child may be at greater risk for Brown syndrome if another member of your family has it.
Symptoms of congenital Brown syndrome
Brown syndrome most often affects only one eye. In rare cases, both eyes are affected. The symptoms can range from mild to severe.
If Brown syndrome affects the right eye:
If Brown syndrome affects the left eye:
-
Your child may not be able to look up with the left eye when looking to the right.
-
Your child’s eyes are often lined up with each other when your child is looking straight ahead.
-
The affected eye might be looking at a slightly lower place than the other eye.
Other signs and symptoms of Brown syndrome include:
-
Double vision
-
Eyes not lined up (in alignment) with each other (called strabismus)
-
Droopy eyelid (ptosis)
-
Chin up and tilted head, which can help a child focus with both eyes
If these problems are present from birth, they are often constant. They may improve over time.
Diagnosing congenital Brown syndrome
Diagnosis begins with a health history and physical exam. This includes a thorough eye exam. It can be hard to diagnose Brown syndrome in a young child. This is because they may not be able to respond to instructions from a healthcare provider during a normal eye exam. Your child may need to see an eye doctor. Your child may also need imaging tests. These can help give more information about the superior oblique muscle tendon.
Treatment for congenital Brown syndrome
Treatment of Brown syndrome may vary based on how severe the symptoms are. If your child has only mild symptoms from Brown syndrome, they may not need any treatment right away. Alignment of the eyes may improve with age.
More severe cases of Brown syndrome may need surgery. Your child may be more likely to need surgery if their eyes are out of alignment when looking straight ahead. Your child might also be more likely to need surgery if they have double vision, or if your child has a very abnormal head position. During surgery, the surgeon cuts the superior oblique muscle tendon and uses a device to lengthen it. This can allow the muscle tendon to move normally. The surgery is usually successful, but some children need repeat surgery.
Follow-up care
Keep track of your child’s symptoms. They will need close follow-up care. If symptoms get worse, take your child to the healthcare provider.