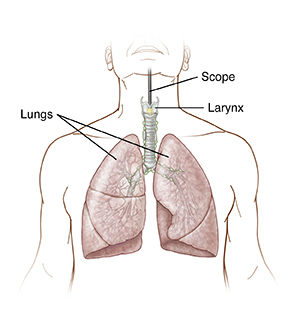
Direct Laryngoscopy with Bronchoscopy
Laryngoscopy and bronchoscopy are two procedures that may be done together. They let the healthcare provider see inside the air passages in the throat and lungs. A laryngoscopy looks at the throat and larynx, or vocal cords. Bronchoscopy looks at the airways including the trachea (windpipe), bronchi, and bronchioles. These procedures can be used to diagnose and treat certain problems. They can also be used to remove objects stuck in your throat or airways. A small tissue sample may be taken for testing (biopsy). Certain problems, such as cysts or scarring, may also be treated. Your healthcare provider will tell you more about your procedure based on why it's being done.
Preparing for the procedure
Prepare for the procedure as you have been instructed. Be sure to tell your healthcare provider about all medicines you take. This includes over-the-counter medicines, herbs, and other supplements. You may need to stop taking some or all of them before surgery. Your healthcare provider will tell you what to stop. Also, follow any directions you’re given for not eating or drinking before surgery.
The day of the procedure
The procedure takes 15 to 60 minutes. Before the procedure starts:
-
An IV (intravenous) line is put into a vein in your arm or hand. This line delivers fluids and medicines.
-
To keep you free of pain, you will be given anesthesia. This may be sedation, which makes you relaxed and drowsy. Local anesthesia may also be injected or sprayed into your throat to numb it. If you are in the hospital, you may be given general anesthesia. This allows you to sleep comfortably through the procedure.
During the procedure
Here is what to expect during the procedure:
-
A tube with a light and a camera, called a scope, is used. The tube may be flexible or rigid. If a flexible scope is used, it is passed through your nostril or your throat.
-
The scope may be moved through the nostril to the throat and then the trachea, bronchi, and bronchioles. Or it may be moved from the mouth to the throat and then to the airways. The scope may send live images from inside the air passages to a video screen. This lets the healthcare provider examine problems more closely.
-
If needed, a biopsy is done using small tools put through the scope.
-
Other tests or treatments may be done with different tools put through the scope.
After the procedure
You will be taken to the PACU (post anesthesia care unit) to be closely monitored as you awake from anesthesia. You will receive pain medicine as needed. Your throat may feel numb or scratchy. Swallowing may feel strange at first. This will improve within a few hours. When you are released to go home, have an adult family member or friend ready to drive you.
Recovering at home
Once home, follow any instructions you have been given. These include:
-
Take pain medicine as directed.
-
Don't eat or drink until swallowing returns to normal. As soon as you can swallow comfortably, drink plenty of water.
-
Use throat lozenges as advised by your healthcare provider to help ease throat soreness.
-
Rest your voice as instructed by your healthcare provider.
When to call your healthcare provider
After you get home, call the healthcare provider right away if you have any of the following:
-
Chest pain or trouble breathing (call 911)
-
Fever of 100.4° F ( 38° C) or higher, or as directed by your healthcare provider
-
Trouble swallowing that doesn’t improve or gets worse
-
Pain that does not go away even after taking pain medicine
-
Severely hoarse voice
-
Severe nausea or vomiting
-
Bloody vomit
-
Cough that brings up more than tiny specks of blood
Follow-up
Follow up with your healthcare provider, or as advised. Within a few weeks, you will receive test results. Your healthcare provider will discuss these with you on the phone or during a follow-up visit. Depending on what was found you may need further evaluation and treatment.
Risks and possible complications
Risks of this procedure include:
-
Bleeding
-
Infection
-
Swelling or injury of the throat
-
Nosebleed (if the scope is passed through the nostril)
-
Gagging
-
Vomiting
-
Cuts in the mouth, nose, or throat
-
Injury to the teeth
-
Vocal cord injury
-
Breathing problems
-
Collapsed lung (pneumothorax)
-
Risks of anesthesia
Online Medical Reviewer:
Ashutosh Kacker MD
Online Medical Reviewer:
Rita Sather RN
Online Medical Reviewer:
Tara Novick BSN MSN
Date Last Reviewed:
12/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.