When Your Child Has Fifth Disease
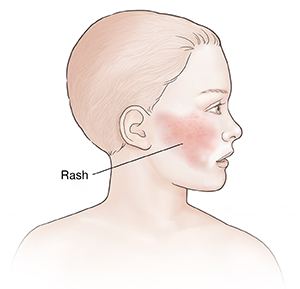
Fifth disease (erythema infectiosum) is a viral infection that is common in children. Fifth disease is also known as slapped cheek disease. This is due to the bright red facial rash that is one of the signs of the infection. Fifth disease usually goes away on its own with no lasting problems.
For pregnant people
Pregnant people should talk with their healthcare provider before having contact with a child who has fifth disease. The virus that causes fifth disease may harm an unborn child.
Why is it called fifth disease?
In the past, erythema infectiosum was number 5 on a list of childhood infections that cause rashes.
What causes fifth disease?
Fifth disease is caused by a virus called parvovirus B19. The virus is spread by droplets in the air when someone who is infected sneezes or coughs. Most children with fifth disease catch it at school or daycare. The virus can spread from person-to-person (is contagious) in its early stages, before the rash appears. Fifth disease is most common in school-age children, but can develop at any age.
What are the symptoms of fifth disease?
 |
| The first rash appears on your child’s face. |
Fifth disease has three possible stages, but many children will have only one or two of them that are noticeable. The stages are:
-
First stage. The earliest stage of fifth disease (the prodromal stage) consists of a low fever, headache, sore throat, muscle aches, chills, or respiratory symptoms. This often looks like a mild cold. Your child may feel tired, cranky, or rundown. This stage may come and go before you notice it.
-
Second stage. This is when the facial rash appears. It is a few days to a week or more after the prodromal symptoms. The rash appears bright rosy red on the cheeks. Your child may also look pale around the mouth because the cheeks are so red. This first rash fades in a few days.
-
Third stage. A rash appears on your child’s arms, legs, and torso. This second rash is flat, purple-red, and looks lacy. It is painless, but may be slightly itchy. The second rash may take 1 to 3 weeks to go away entirely. It may get better or worse during this time.
How is fifth disease diagnosed?
Your child's healthcare provider may do a blood test to check for the virus. However, it is usually diagnosed by the appearance of the distinctive rash. In some cases, tests may be done to rule out other health problems.
How is fifth disease treated?
Fifth disease needs no treatment. It will go away on its own. To help your child feel better until it does:
-
Be sure they get plenty of rest and fluids.
-
Your child’s healthcare provider may suggest giving children’s strength over-the-counter (OTC) medicines to help relieve fever or discomfort. Note: Don’t give OTC cough and cold medicines to a child younger than 6 years old, unless your child's provider tells you to do so.
-
Don’t give your child aspirin. Giving aspirin to children younger than age 19 may cause a serious condition called Reye syndrome. This condition affects the liver and brain.
-
Don’t give ibuprofen to an infant age 6 months or younger.
-
An anti-itch medicine called an antihistamine may be recommended if the rash is itchy.
Returning to school
Once your child develops the rash, they are no longer contagious and may go to school or daycare. A child who still has a fever should not go to school or daycare.
What are the long-term concerns?
Once your child has had fifth disease, they will usually not get it again. Fifth disease rarely causes problems in children who are otherwise healthy.
When to call the healthcare provider
Call your child’s healthcare provider right away if your child has any of these:
-
Fever (see Fever and children below)
-
Severe muscle or joint aches and pains with the rash or fever
-
Rash that doesn’t clear up after a few weeks
-
A weak immune system for any reason
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider